OC 949-428-4500
LA 310-460-2444

We call them rashes and eczemas. Some are caused by genetics, others by lifestyle factors, and many are linked with allergies. Most are treated with the aid of topical corticosteroids and constant skin moisturizing.
Yet, after all is said and done, how much do we really know about the different types of dermatitis out there? What are they? What causes them? Can they be prevented? Read on, to learn more about the seven most often encountered types of dermatitis.
Many unknown facts remain to be discovered about the most frequently observed type of dermatitis, atopic dermatitis, most commonly referred to as eczema. Modern medical science has yet to discover just what causes it and how it can be cured. However, given its prevalence (28 million Americans are estimated to suffer from it), it’s definitely worth discussing.

No two eczemas are the same, but they all share certain core symptoms:
The precise cause of atopic dermatitis remains unknown and is likely a combination of genetics and environmental triggers. Here are some of the most often mentioned probable causes of eczema:
Some 10 to 15% of babies develop eczemas before the age of 1. Though the condition usually goes away on its own, most often between a child’s 8-month and 2-year birthday, it’s important to know how you can stop the condition for worsening. While all the other advice below applies, remember that you have to prevent the child from scratching. Keep their nails trimmed short, consider filing them, and even use mittens or cotton socks on their hands, to keep them from drawing blood through excessive scratching.
Most mild cases of eczema can be helped through good skin care and a few lifestyle modifications. And these will even prove helpful for more severe cases.
Here is what you should do:
If your rash is particularly severe, you’re going to need a prescribed treatment. This usually involves one or more of the following:

Seborrheic dermatitis is also known by a lot of other names – but the most common one is simply dandruff. Medical professionals may refer to it as cradle cap, seborrhea, seborrheic eczema, sebopsoriasis, and pityriasis capitis.
It’s an inflammatory disorder of the skin, with typically mild manifestations, that is more prevalent in men than in women. It is estimated that more than 50 million people suffer from Seborrheic dermatitis in the U.S.
It causes scaly skin and looks a lot like a common allergy, as well as psoriasis, and eczema. Though seborrheic dermatitis differs in its manifestation from one case to the next, certain symptoms are common to most cases:
As is the case with eczema, we don’t know for sure what causes seborrheic dermatitis. It can be any number of factors, or rather a mix of them, selected from the non-exhaustive list below:
Certain medications and conditions can also cause seborrheic dermatitis:
The first steps to follow, in terms of treatment, entail self-care. But, when all else fails, and you’re losing sleep or are having trouble concentrating because of seborrheic dermatitis, it’s time to see a doctor. Here’s what you can expect them to prescribe:
Judging by the name of this condition, you might think that it has something to do with one of the several known strands of the human herpes virus. In fact, dermatitis herpetiformis, which is also known as Duhring’s Disease, only shares the blister-filled skin inflammation aspect of herpes.

As with all types of dermatitis, the main issue caused by this condition is an intense desire to scratch the severe itchiness it causes. Here are some other symptoms of dermatitis herpetiformis:
Chronic blisters. These are usually located on extensor surfaces: buttocks, back, knees, groin, face, scalp, elbows, etc. They are symmetrically disposed and range from minuscule sizes to up to 1 cm in diameter. The only mucous membranes on which they typically appear are the mouth and lips – and even this is a comparatively rare occurrence.
As with many other skin conditions, the exact causes of this disease remains unknown to this day, even though it was first discovered by Louis Duhring in the late 19th century. What we do know about the causal mechanism of this condition can be found below:
It’s essential to get a proper medical diagnosis for this condition, since, not only does it accompany another life-changing disorder, but it can easily be confused for something it is not. Such typical mix-ups include contact dermatitis, drug rashes, dyshidrosis, even scabies.
To get a sound diagnosis, your blood needs to be tested for IgA antibodies, and you also need a biopsy revealing IgA deposits. The disorder is usually treated with dapsone, which reduces the itchiness over the short span of 2-3 days. However, this drug will not take care of any other symptoms of coeliac disease. Interestingly enough, it remains unclear how the anti-bacterial dapsone can prove effective in treating a disease not caused by bacteria. At the same time, such treatment also leaves you vulnerable to blood conditions. As a sufferer of coeliac, you are going to have to maintain a strict gluten-free diet, possibly for the rest of your life. In time, as the symptoms are likely to diminish, feel free to stop the dapsone dosage, as per doctor instructions.
Bear in mind that this an autoimmune disease, so you are also likely to be suffering from associated conditions, such as lymphoma in the intestines and thyroid issues. Due to its autoimmune character, an exaggerated immune response is likely pointing to other malfunctioning areas, not related to digestion.
Finally, since this disorder is a manifestation of coeliac, you are also more prone to certain types of gut cancer, thyroid disease, and osteoporosis.

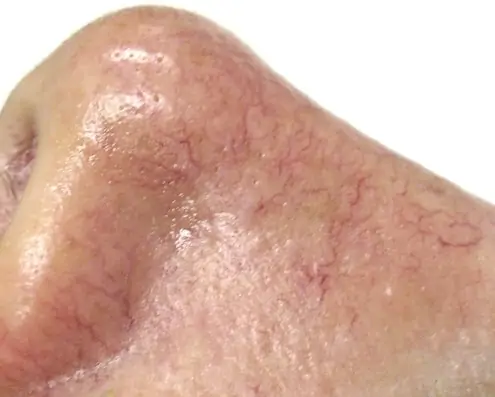
You already know a lot about this condition, at least where its main symptom is concerned. You touch something and your skin turns red, immediately becomes tender, and is frequently also sore. Your name for it is likely to be ‘rash’, but the proper medical term is contact dermatitis.
As you’ll learn below, there are some differences between the two main types of contact dermatitis. However, they are similar in their manifestation, as follows:
There are two main causes for contact dermatitis, as outlined below:
1. As with all allergic reactions, coming into contact with a particular substance will cause your body to think it is being attacked. This, in turn, will trigger an immune response, which generates antibodies as a protective ‘shield’. The final link in this chain of events is the production of histamine, which is actually what results in an itchy skin condition, i.e., the rash. Some of the most frequent triggers of allergic contact dermatitis are:
Poisonous plants, such as sumac, ivy, and oak.
It is never the case that you develop contact dermatitis from the first time you touch a triggering substance. If you believe that you do, it’s likely because you’ve touched that trigger before and your skin has already been sensitized to it – but you were simply not aware of it. Allergy contact dermatitis develops a couple of days after coming into contact with the allergen.
2. Damaged skin. This particular type of rash is called irritant contact dermatitis. It might look a lot like an allergy, but the rash in this case is actually caused by damage to the skin, which removed its protective oils. It was caused by prolonged contact with that substance and involves no immune response. Some of the most common triggers of irritant contact dermatitis, which is also known as hand eczema are:
These rashes show up immediately. If you suffer from eczemas, you are more prone to this type of rash.
A third, but far less common type is photo-contact dermatitis, in which the rash is caused by the active ingredients in sunscreen react when exposed to the light of the sun.
There are a few self-care steps that you can do at home. However, if a couple of days have gone by and the rash still isn’t subsiding, do call your doctor. They will likely:
As for self-care, here’s what you can do in the initial stages of the rash, on your own, at home:
The name of this condition will tip you off to just what it is: a rash that develops around the mouth. It is most frequently seen in women, who make up 90% of sufferers. However, it can also be experienced by men, too.

Perioral dermatitis is part of the family of very similar conditions, each known by a specific name, based on the area where the papules (blisters) emerge:
The rash can sometimes spread to the nose and forehead. It is usually accompanied by a burning sensation around the mouth. Here are it’s most common symptoms:
Although perioral dermatitis resembles rosacea induced by steroids, unlike that condition, it does not emerge on the cheeks.
Contemporary medical science doesn’t know what causes perioral dermatitis. However, certain correlations have been established with:
Perioral dermatitis can usually be diagnosed straightforwardly, without any need for specific tests. It can be treated fairly easily and takes some two weeks before it is fully healed.
To avoid contracting this condition, you should also avoid using any creams that might clog your pores or effectively block your skin. Also, if you’ve been prescribed topical corticosteroid creams for other conditions, apply them only to the affected areas, no more often than twice a day, and in the lowest concentration specified in the prescription.
If you’ve contracted perioral dermatitis, you will first need to take some measures to prevent it from spreading or aggravating:
For mild cases, your doctor will likely prescribe a topical lotion, such as erythromycin, azelaic acid, pimecrolimus, metronidazole, or clindamycin. For more severe cases, you might have to follow a 6 to 12 week antibiotic treatment of tetracycline (doxycycline) in sub-antimicrobial doses. Pre-pubescent children and pregnant women are usually prescribed oral erythromycin. If, for whatever reason, antibiotics are not an option, your doctor might prescribe a low dose of oral .

If you’ve got poor circulation in your legs and, especially if you’re overweight, very sedentary, and over 50, you’re likely to develop this fairly common skin condition. Heart disease is also a factor that puts you at increased risk. How can you avoid developing stasis dermatitis? Simply sit less. By doing so, you avoid developing swollen lower legs, or peripheral edema. Though stasis dermatitis is not uncommon, complications in severe cases can lead to skin ulcers.
Sufferers will typically experience both symptoms of stasis dermatitis and venous insufficiency simultaneously. Those in the former category include:
If you’re affected by venous insufficiency, you might experience:
Early on, with the onset of stasis dermatitis, you might see thinner skin on your legs and experience itchiness. Try not to scratch it, as this will cause lesions and oozing. With time, your skin might turn brown, become thickened, lumpy, or hardened. Eventually, in the late stages of the condition, your skin will break into sores or ulcers. These sores usually appear on the inside of the calf.
Women tend to be more affected by stasis dermatitis than men—especially those who meet the criteria listed above. Here’s what causes the condition: blood tends to accumulate in the lower part of the legs. This, in turn, will increase blood pressure in the veins. The smallest of those vessels, i.e., the capillaries, will break and leak protein into the tissue. This is why your legs swell, or why you develop peripheral edemas.
One of those proteins leaked into the tissues is fibrinogen. Though no direct link has been established between the presence of this protein in the tissue and stasis dermatitis, it is the one directly responsible for the creation of fibrin cuffs. They effectively cut off oxygenation to the tissue, thus damaging and eventually killing cells.
Here are some common risk factors for developing this type of dermatitis:
Also, the more you sit, the more likely you are to develop swollen legs and, in turn, stasis dermatitis. For most people, these risk factors increase as they age.
If you’re experiencing pain, ulcerated skin, and oozing, it’s definitely time to see a doctor. Aside from examining the skin on your legs, they will order a Doppler ultrasound, which checks blood flow to the legs via sound waves.
To prevent the aggravation of this condition, you can:
To help alleviate the symptoms of stasis dermatitis, your doctor might recommend one or several of the following:
It’s important to address this condition, before it aggravates and turns into permanent scars, bacterial infections of the skin, bone infections (osteomyelitis), and chronic leg ulcers.
This condition derives its name from the Latin word ‘nummus’, i.e. ‘coin’. In a similar vein, it’s also known as discoid dermatitis. Both these facts are actually references to the main symptom of nummular eczema.

Nummular neurodermatitis, as the condition is alternatively known, is chronic and most often found in aging men, past 60-years-old. It is manifested through the appearance of round, coin-sized patches of skin that become itchy, dry, scaly, and discolored. They most often emerge on the buttocks and legs, although they can appear anywhere on the body.
People with dry skin are particularly affected by this condition and dry, cold climates are particularly conducive to the emergence of the disease.
The condition is not genetically determined, it’s not linked to any dietary allergens, nor can it spread from one person to another. It is usually caused by dry weather and aggravated by any factor that contributes to the drying of the skin: stress, excess caffeine intake, and other dehydrating agents.
To help diagnose the condition, your doctor is likely to examine the skin and possibly order a patch test. It can be treated at home, especially through making sure the skin is properly moisturized at most times. To this end, non-irritating creams, lotions, and bath oils are recommended. In more severe cases, doctors will prescribe topical corticosteroid creams, oral antihistamines, and even UV light therapy.
Doctors Alice Pien, MD and Asher Milgrom, Phd are established pioneers in the fields of Regenerative Medicine and Skincare. Their expertise ranges from advanced laser systems to HCT/P – Stem Cell medicine. Their medical education and advanced certifications span from medical schools of NY State University, the University of Chicago, to Johns Hopkins, Harvard and UCLA. They approach medicine with the clinical expertise of over 85,000 successful treatments over the past 20 years and significant scientific research resulting in proprietary protocols that they customize for each individual patient.
AMA Regenerative Medicine & Skincare | 1570 Brookhollow Dr., Santa Ana, CA 92705 | 6310 San Vicente Blvd STE 285, Los Angeles, CA, 90048 | Privacy Policy