
OC 949-428-4500
LA 310-460-2444

As the cases of Long COVID continue to increase, it is important for the medical community to begin focusing on long-term therapeutic strategies that target the chronic ischemic and inflammatory environment seen in the brains of those infected or previously infected by COVID-19.
One of the pharmacological agents that the medical community is starting to take notice of for this purpose is Methylene Blue.
Methylene Blue (MB) has a long history of use, although it has not always been utilized for pharmaceutical purposes. It was first synthesized in 1876 for use as a textile dye, but as early as 1891, it was investigated for its medicinal applications. One of its first applications in the medical field was as a medical strain, but it soon expanded to be used in treatments.
Its classic uses in the medical field include treatment for malaria, carbon monoxide poisoning, and methemoglobinemia. However, its effect on mitochondria has been receiving growing interest. There is also growing interest in the connection between mitochondrial dysfunction and Long COVID symptoms, adding to the appeal of MB as a potential pharmacological agent and treatment.
MB plays a significant role in the mitochondria due to its ability to act as a catalytic redox cycler. This mechanism allows it to reroute electrons in the mitochondrial electron transfer chain from NADH to cytochrome c. When this occurs, the activity of complex IV is increased, which promotes mitochondrial activity while mitigating oxidative stress.
Since oxidative damage, which is caused by mitochondrial dysfunction, impairs complex IV, the ability of MB to increase complex IV activity plays an important role in its ability to address and correct mitochondrial dysfunction.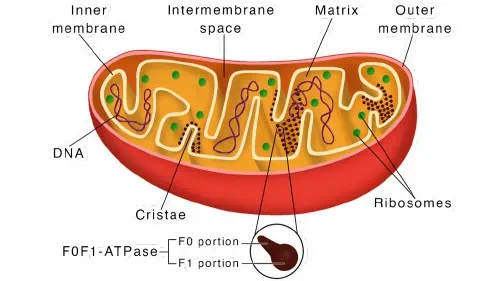
Because of MB’s ability to influence the mitochondria and increase their functioning, it is important to consider what the role of the mitochondria is, and why their dysfunction plays a central role in Long COVID symptoms.
The mitochondria are organelles that generate most of the adenosine triphosphate (ATP) used by the cell. Virtually every ounce of energy generated in your body comes from the Krebs Cycle and the Electron Transport Chain both found in the mitochondria.
Virtually every biochemical reaction requires the input of energy in the form of ATP. Without ATP all it takes is six seconds for the cell to start deteriorating. The first thing that deteriorates in the cell without ATP is the mitochondria Itself.
Some of the other cellular biological processes in which mitochondria play essential roles include apoptosis, calcium signaling, cell growth, reactive oxygen species (ROS) generation, and cell cycle.
The mitochondria are very often denoted as the “powerhouse” of the cell due to their role in ATP production, but the truth is that they play a much more important role in the body, particularly affecting immunity.
The mitochondria sense the cellular environment and control inflammation, growth, senescence, and death. With these roles, the mitochondria balance metabolic priorities between growth, energy production, defense, and oxidative stress management. There are many tasks handled by the mitochondria, and having a good mitochondrial reserve ensures that the cell can remain flexible and multi-task. The loss of this flexibility can contribute to aging-related changes in the immune system.The average cell in the human body has between 1000-2000 mitochondria depending on the metabolic energy it needs to:
In contrast, cardiomyocyte cells have 6-8000 mitochondria, and neurological cells are by far the most metabolically active cells in human physiology and contain on average between 2 – 3 million mitochondria in order to:
Given the vital importance of mitochondria as the generator of all of your biochemical “life” energy, that without healthy mitochondria your damaged neural network cannot be repaired.
Mitochondrial dysfunction occurs when there is a loss of function in mitochondria, and is a common observance in many neurological disorders that possess both chronic and acute neural injury. Some diseases that show mitochondrial dysfunction include neurodegenerative diseases and brain injuries from a lack of blood and oxygen supply.
Mitochondrial dysfunction plays a role in the induction of factors that lead to brain disorders, such as inflammation, oxidative stress, transcriptional alterations, and excitotoxicity. For neurological disorders such as traumatic brain injury, Alzheimer’s disease, depression, Parkinson’s disease, and stroke, mitochondrial dysfunction contributes to the disease’s pathophysiology because of decreased energy production and excessive reactive oxygen species (ROS) production. Excessive ROS production leads to oxidative stress, which is a major contributing factor to many neurodegenerative diseases.
Further studies into the effect of mitochondrial dysfunction on these neurological disorders have found that restoring mitochondrial function may serve as a treatment method, with many studies showing improvements in brain mitochondrial function after treatment for the neurological illness.Studies have found that COVID-19 can directly or indirectly affect the central nervous system (CNS). These effects on the CNS can contribute to the symptoms seen in those with long-COVID, such as serious long-term mental and cognitive changes, including “brain fog.”
With infection, the SARS-CoV-2 RNA genome integrates into the host mitochondrial matrix, which leads to virus replication and increased viral load
The viral RNA then hijacks the mitochondrial function to suppress the body’s immune response and further promote viral replication. As the infection continues, the infected cells (which can include neurons) may experience oxidative stress and calcium ion influx that can lead to necrosis, apoptosis, or dysfunction, along with impaired mitochondrial function.
The tissues in the brain require an immediate and constant supply of oxygen to keep up with their significant metabolism. However, the SARS-CoV-2 virus may cause hypoxia in some regions of the brain to benefit its reproductive abilities. This hypoxia can then compromise neuronal cell energy metabolism, leading to mitochondrial dysfunction in the cerebral tissue.
This theory of the effect of the SARS-CoV-2 virus on the CNS has been confirmed with autopsies showing the presence of the coronavirus in the CNS, especially in the brain.
SARS-COV-2 infects cells through its spike protein, which binds to a surface receptor on the target cell. Many people who have been infected will develop antibodies that neutralize the spike protein. However, those who produce antibodies that neutralize one COVID-19 strain but not another are known to have increased chances of antibody-dependent enhancement (ADE) to the new strain, which may explain Long COVID symptoms.There’s more to the spike protein than its ability to let the virus connect to a target cell, though, with the spike proteins themselves being toxic to human physiology. Free spike protein can have several direct pathologic actions on cells, including stimulating pro-inflammatory and vasoactive mediators, especially platelet-activating factors.
The spike protein can also damage the blood-brain barrier (BBB) and change its function by inducing the inflammatory response of microvascular endothelial cells. These findings support the observances that SARS-CoV-2 can alter the BBB and pass through it to enter the brain. The SARS-CoV-2 spike protein-binding receptor (ACE2) is also widely expressed in brain microvascular endothelial cells, which is why it often targets these cells, causing inflammation and the neurological symptoms associated with COVID-19.
Not only does the observance of the spike protein damaging and passing through the BBB support clinical reports detailing early neurological changes, but it also serves as a basis for long-term neurological symptoms.Those with a COVID-19 infection can show neurologic symptoms such as:
Some of these symptoms are common in other neurological conditions, such as Alzheimer’s disease, multiple sclerosis, and Parkinson’s disease, causing those with Long COVID to be potentially misdiagnosed because of the mimicking of symptoms. Additionally, there is a growing concern about the long-term effects of SARS-CoV-2 on the CNS and cognitive function. Specifically, if SARS-CoV-2 causes neurodegenerative diseases or if it accelerates their occurrence prematurely.
Research also shows that the spike protein can have these same effects from other sources of the spike protein, not just from the infection itself. A 2021 study found that those with Long COVID and who had obtained the spike protein from another source both showed retained spike protein in monocytes.
Additionally, this study examined patients who showed symptoms of Long COVID after being given the spike protein and found that they responded to treatments intended for Long COVID, supporting the observance that other sources of the spike protein can cause Long COVID.
Studies also show that the spike protein from other sources selectively and potently drives pro-inflammatory cytokine secretion in human monocytes. This supports our belief that the spike protein is causing the inflammation and mitochondria problems seen in those with Long COVID, and this research explains why we are seeing patients with similar symptoms no matter if they got the spike protein from the infection or from another source.A significant amount of evidence shows that changes induced by mitochondria, such as oxidative stress, dysfunctional electron transport, Ca2+ imbalance, impaired mitochondrial trafficking, defective mitophagy, and altered mitochondrial dynamics, show some involvement in various brain diseases.
Since MB is able to correct mitochondrial dysfunction, it shows promise as a treatment for Long COVID. It can target and improve many areas of mitochondrial damage, although the two most notable areas in regard to Long COVID treatment include oxidative stress and neuro-inflammation because they have the greatest impact on neurons.
The benefits of MB on other neurological diseases that are related to mitochondrial dysfunction, such as stroke and Parkinson’s disease, have been well documented. We have also seen improvements in our patients when treating Long COVID with MB, further supporting the use of MB to correct cases of mitochondrial dysfunction for those with neurological conditions.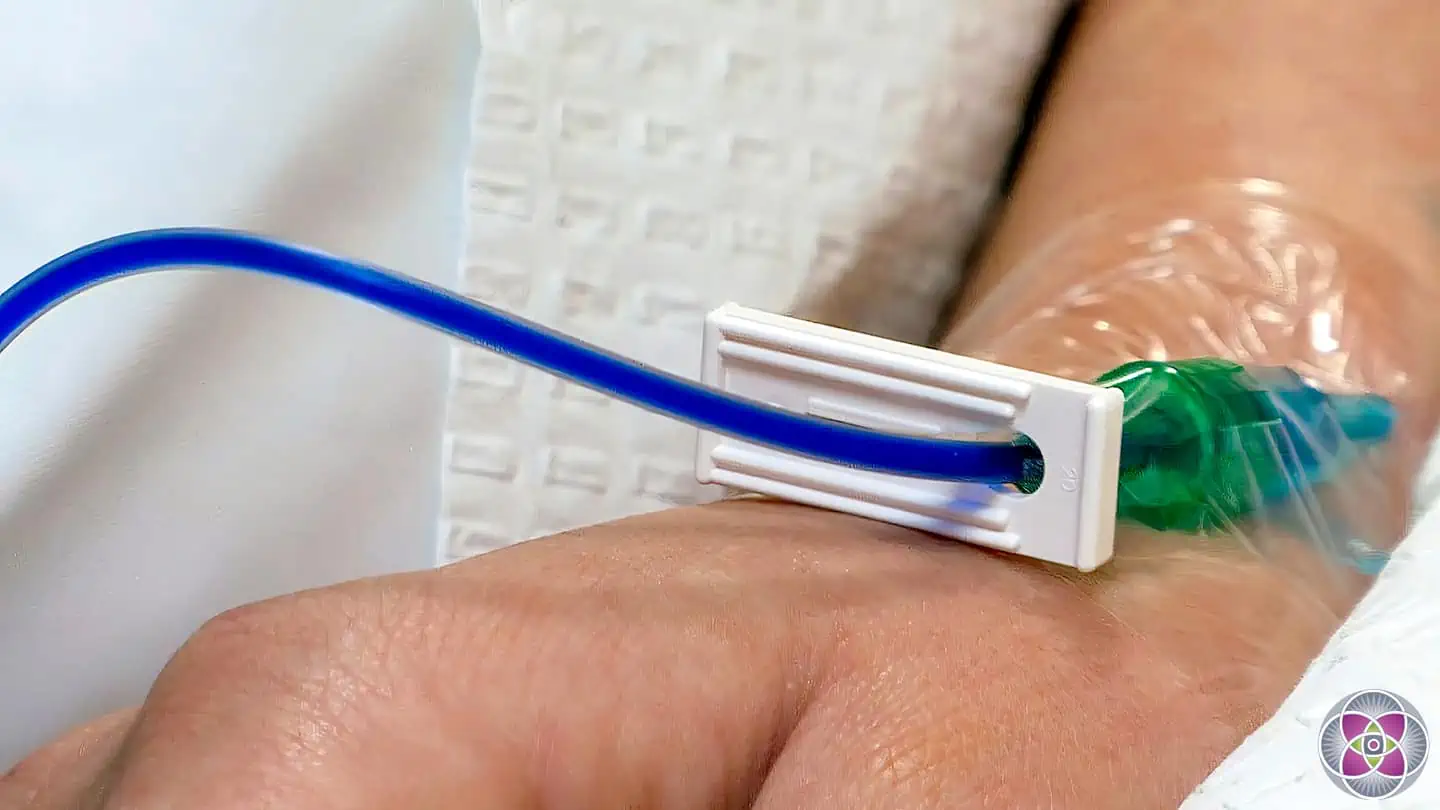
The ideal method for administering MB is intravenously since it allows for a higher available drug concentration compared to oral delivery.
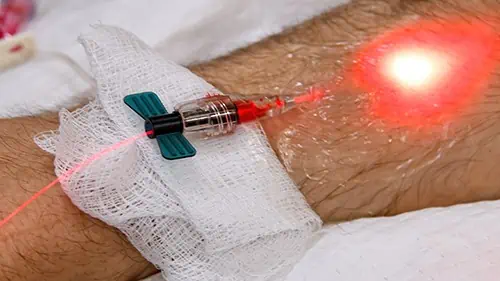
Once administered, MB accumulates in tissues at significant concentrations. This includes the brain tissue, and the high concentration allows it to cross the BBB and potentially enter neuronal mitochondria. However, the mechanism by which it penetrates mitochondria remains unclear.In general, photobiomodulation (PBM) and photodynamic therapy (PDT) are two primary methods, which use light in medicine and dentistry.
Due to similar, but not fully understood mechanisms and biphasic response of light, unexpected and complex outcomes that as yet defy explanation may be observed. Thus, step-by-step protocols have yet to be developed that produce thorough, reliable, and reproducible results for a majority of conditions.
What is clear however, is that the low-level energy of the lasers and LED light being used are safe and easy to use.
Regarding COVID, both of these modalities should theoretically be useful, perhaps even critically important if they can be combined.
We need to kill the virus as soon and as quickly as possible. For this, Photodynamic Therapy with a Photosensitizing agent that can target and become concentrated in the virus, and a laser with a corresponding frequency of energy (wavelength) that is readily absorbed by the Photosensitizing agent.
The energized Photosensitizing agent will now release ROS that are deadly to the virus. Ideally a properly constructed protocol that takes advantage of these properties will clear a patient of an entire viral load quickly, and before systemic damage is created.Photobiomodulation (PBM) is another therapeutic approach targeting mitochondria, but its underlying mechanism differs from MB. Because of these differences in mechanisms, combining PBM and MB can offer better results than either therapy individually.
PBM is also known as low-level laser therapy and involves the application of red-beam (400-720 nm) or near-infrared (700-1000 nm) laser on biological tissues. PBM can modulate various biological processes due to its ability to target the mitochondria. The low-level laser donates photons to complex IV, which increases its activity and thus oxygen consumption.
Growing research on the effect of the SARS-CoV-2 spike protein on mitochondrial dysfunction, and thus the role of the mitochondria in Long COVID symptoms, has led to an increasing need for pharmacological treatments that repair the mitochondrial function.
Methylene blue is a pharmacological agent showing appealing results as a treatment for Long COVID, which we suspect is due to its ability to correct mitochondrial dysfunction. When combined with photobiomodulation, another therapeutic approach targeting mitochondria, the treatment becomes even more effective.Everything on our website comes from from reputable publications, books and scientific journals, most of which are available on PubMed and other government websites. These include Meta-Analysis’, Randomized Controlled Trials, Clinical Trials, Systematic Reviews, Books and Documents. We encourage you to read the science, in order to separate fact from fiction, so that you can arrive at a full understanding of what is best for your body. We would be honored to be a part of that educational journey with you.
AMA Regenerative Medicine & Skincare | 1570 Brookhollow Dr., Santa Ana, CA 92705 | 6310 San Vicente Blvd STE 285, Los Angeles, CA, 90048 Disclaimer: though everything on our website comes directly from reputable publications and scientific journals; and though thousands of these articles are available on official government websites (https://pubmed.ncbi.nlm.nih.gov), they have not been evaluated by the Food and Drug Administration and the FDA has not certified, endorsed or approved any of the scientific findings as methods of treating or diagnosing any diseases or illnesses.