
OC 949-428-4500
LA 310-460-2444
As more and more individuals are infected with, and then recover from COVID-19, the number of people who then fall victim to Long COVID also increases. One of the most common symptoms of Long COVID is profound fatigue, affecting 58% of those with Long COVID, according to a 2021 meta-analysis. Fatigue is a debilitating symptom that affects all aspects of our lives, including our concentration, relationships, and ability to work, in addition to generally decreasing our quality of life.
Not only is fatigue one of the most common symptoms of Long COVID, but it is also a symptom that lasts for a long time, present even 100 days after the first symptom of acute COVID-19 in some individuals. In one study, two-thirds of the sample had chronic fatigue more than six months after their initial COVID infection.
Identifying the cause of Long COVID fatigue is challenging, with no identifiable relationship between the development of fatigue, COVID-19 severity, and level of inflammatory markers. What is interesting is fatigue is more common in females and those diagnosed with depression or anxiety.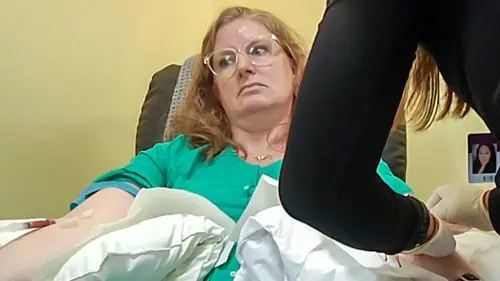
The fatigue and symptoms seen in Long COVID patients are very similar to Chronic Fatigue Syndrome. Shared symptoms include:
Despite the similarities in Long COVID and Chronic Fatigue Syndrome, many patients are told by their PCP that the symptoms negatively impacting their life are caused by anxiety or depression.
Long COVID fatigue is a very real symptom. In fact, it affects more than half of those with Long COVID. It is NOT just in people’s head.
The fatigue experienced by those with Long COVID is often described as more than just feeling tired. It is as if their life-force has been completely drained from them. Many people with Long COVID fatigue describe both mental and physical components and a worsening of the fatigue after only a minor physical or cognitive activity.Reported symptoms of mental fatigue include:
The physical fatigue experienced by those with Long COVID makes it difficult to perform physical activities because of a loss of energy and/or feelings of heaviness.
Those with Long COVID experience fatigue that is reported to be equal to, or higher than, other chronic diseases including Chronic Obstructive Pulmonary Disease (COPD), Q Fever, Asthma, Rheumatoid Arthritis, Multiple Sclerosis, and Systemic Sclerosis. What makes this even more unprecedented is the number of otherwise healthy individuals suffering from Long COVID fatigue without the presence of other co-morbidities.A 2021 study sought to interview people who suffer from Long COVID fatigue to better understand their personal experiences and perceptions. One respondent said that Long COVID fatigue feels most like weakness,
“I’m so tired. I am weak both while lying down and working.”
Yet another explained how it has theoretically aged their body,
“I am 30-years-old, but my body is like a 70-year-old.”
The mental effects of fatigue were also present in the individuals included in the study,
Social lives are also significantly impacted by Long COVID fatigue, with many responders explaining that after doing any work or housework, they have no remaining energy for socializing. Even talking to someone tires them out. There’s a desire to go out and see friends and family, but the fatigue experienced makes that seem impossible.“I always forget. I say something, then forget it. I do something, then forget it.”
Fatigue is a common symptom across many chronic viral and bacterial illnesses, including Ebola, EBV, Influenza, Epstein-Barr , and Lyme. Unfortunately, those experiencing chronic fatigue from these conditions have likely been ignored and forced to suffer with their chronic fatigue for years or even decades. However, because of the similarity between these illnesses and Long COVID, those with other viral and bacterial illnesses can benefit from pandemic-related research.
The pandemic has resulted in increased research on chronic infections and post-viral syndromes in general, providing more information on all diseases falling into this category, not just Long COVID. While there are a lot of negative repercussions caused by the pandemic, this is one of its silver linings since any research in the field of chronic fatigue is a step forward.Studies are showing five promising treatments for Long COVID fatigue. We are also seeing the success of these treatments in our clinic.
Below we provide a brief overview of each treatment and the studies supporting its benefits.

The benefits of high-dose IV vitamin C for fatigue extend from its antioxidant, endothelial-restoring, anti-inflammatory, and immunomodulatory effects.
A 2021 review collected nine clinical studies on Vitamin C treatment in post-viral fatigue with similar markers as Long COVID fatigue, such as inflammation, oxidative stress, and circulatory disorders. There were four controlled trials, and in three of them, there was a significant decrease in fatigue scores between the vitamin C and control groups. The remaining five trials were observational studies, and four of these observed a significant reduction in pre-post fatigue levels.

A patient being treated with the EBOO /F aphaeresis device. Dark, dirty blood comes out of one arm. The blood is filtered, removing any debris, and also infused with ozone by the device. Then the purified, bright red, blood is returned to the other arm.
A 2022 study found that those with chronic fatigue syndrome due to viral or autoimmune pathogenesis, such as Long COVID fatigue, may be linked to receptor antibodies against ß- adrenergic and muscarinic receptors since both of these autoantibodies are elevated in those with Long COVID.
Aphaeresis uses a special filter that, based on current research, appears effective in reducing these antibodies, which then improves symptoms in those with Long COVID fatigue.Hyperbaric Oxygen Therapy (HBOT) is a promising treatment in which the patient is placed in a chamber where the atmospheric pressure is increased while they breathe in pure oxygen. This treatment helps patients with Long COVID intake more oxygen and deliver this oxygen more effectively to the cells and tissues of their body.
A 2021 study on HBOT for Long COVID evaluated the effect of HBOT on ten patients, recording their fatigue scale. The results showed a significant improvement in fatigue, global cognition, executive function, attention, information profession, and verbal function.

Methylene Blue works wonders on CV19, Long COVID, Epstein Barr and Lyme disease patients. These diseases damage the mitochondria causing their Electron Transport Chain to stop working properly. Your mitochondria are no longer able to make ATP which is the primary energy source for important biological functions.
Stopping the production of ATP causes the cell to essentially become senescent. It’s trying to live, it’s trying to die, it doesn’t know what to do, it doesn’t have the energy to do anything, so it just hangs around. Now imagine this happening to all 50 trillion or so cells in your body… Fatigue unlike anything you have ever experienced.When Methylene Blue is put into the body and enters the cell, it bypasses the part of the Electron Transport Chain that has been damaged and donates electrons directly into ATP synthase at the end of Electron TransportChain.
Now the mitochondria can make ATP with a source of electrons that has not been cut off and the cell can now repair itself. This is what we believe is happening inside the body and the clinical results we are achieving with our patients reinforces this.
The point is that with Methylene Blue your body can repair itself, using the ATP produced by your own mitochondria, giving your own cells the energy they need to repair themselves.Whole body cryotherapy exposes a patient to extremely cold and dry air for two to three minutes. This provides benefits such as vasoconstriction, slower nerve condition, and stimulation of dermal thermo-receptors. It is currently used in inflammatory conditions such as Fibromyalgia, Rheumatoid Arthritis, and Ankylosing Spondylitis.
In January 2022, a hospital in Italy detailed a case report of cryotherapy for Long COVID on a 75-year-old patient. Immediately following his first session, he reported immediate improvements in breathing, and the following hours showed improvement in sleep quality and a reduction of weakness. From this point on, the patient reported lower fatigue.
Supplements can help reduce inflammation or address deficiencies seen in those with Long COVID fatigue. Omega-3 fatty acids, vitamin D, curcumin, vitamin C, melatonin, kefir, and probiotic yogurt can all help reduce both mental and physical fatigue.
However, to see a benefit, the correct dosage should be taken. The FLCCC protocols include guidance on how much of each supplement to take.Long COVID’s most common and debilitating symptom is fatigue, affecting patients both mentally and physically and leaving them feeling exhausted, unlike themselves, and unable to gather the energy to function in life. It’s a condition often brushed aside, but the numerous studies investigating it, and the countless people experiencing it, have proven that it is a very real condition and one that can continue to impact individuals months and even years after their initial COVID diagnosis.
Based on prior research and results within our clinic, there are six promising treatments for long COVID fatigue: ozone therapy, high-dose IV vitamin C, aphaeresis, HBOT, Methylene Blue, whole body cryotherapy and the list keeps on growing. NAD is another promising therapy. These therapies have significantly reduced fatigue in our patients, sometimes curing someone of fatigue completely. This is why, in our eyes, they remain promising treatments for long COVID and other post-viral fatigues including Post Vaccine Syndrome.Everything on our website comes from from reputable publications, books and scientific journals, most of which are available on PubMed and other government websites. These include Meta-Analysis’, Randomized Controlled Trials, Clinical Trials, Systematic Reviews, Books and Documents. We encourage you to read the science, in order to separate fact from fiction, so that you can arrive at a full understanding of what is best for your body. We would be honored to be a part of that educational journey with you.
AMA Regenerative Medicine & Skincare | 1570 Brookhollow Dr., Santa Ana, CA 92705 | 6310 San Vicente Blvd STE 285, Los Angeles, CA, 90048 Disclaimer: though everything on our website comes directly from reputable publications and scientific journals; and though thousands of these articles are available on official government websites (https://pubmed.ncbi.nlm.nih.gov), they have not been evaluated by the Food and Drug Administration and the FDA has not certified, endorsed or approved any of the scientific findings as methods of treating or diagnosing any diseases or illnesses.